When thirty-four year-old Leanne Molloy found that she had to stand up and ‘jiggle’ her body to get food to go down, she knew she had a problem!
“I suffer from anxiety” Leanne, 35, said: “so when I started to feel that my heart was missing a beat, I had an ECG. Unfortunately, the first lockdown happened and so everything went by the wayside and I didn’t get the results.
“In November, I had a small birthday party for my daughter but when I ate a few chips, I felt something getting caught in my throat.
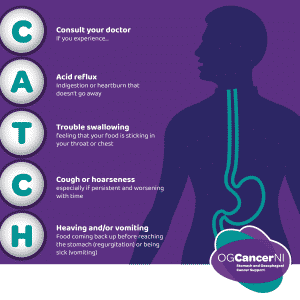
“This started happening on a regular basis. Sometimes I’d eat and be fine, but one evening I was eating soup and bread and I knew there was something wrong. I increasingly had to stand up and ‘jiggle’ my body until I felt the food passing. Sometimes I had to make myself sick just to get it up.
“There were things that I could eat with no difficulty, but other things would stick. I learnt to jiggle my hands up and got my husband to look after our daughter so I could go out of the room and jiggle. I was always a fast eater but I didn’t chew properly, so I began to eat more slowly and not at my husband’s pace. Put simply, I was changing my habits to suit the symptoms, rather than getting the symptoms sorted.
“Over time I spoke to the GP and told him there was pain going into my shoulder blade. I’d also started to lose weight but that’s because I wasn’t eating properly. The GP gave me more tests and then arranged for me to go to the hospital on a Sunday morning for a test. There were so many there I nearly walked out.
“I had the scope but, because I didn’t get sedated, I was aware of what was going on and I noticed that two nurses were going over the notes and talking. Then I was moved into another room and somebody came in and asked for bloods. They also asked me where my husband was. He was in the waiting area. They went and got him and I was called into another room. My husband came in and we looked at each other. When they told me they’d found something, I was so relieved cos I knew there was something. The consultant said they’d found something at the bottom of my oesophagus. I said ‘cancer’? I just came out with it. The consultant said, ‘Yes, it’s looking very like it’. I was just numb.”
Leanne, from Castlewellan, works in a pharmacy and, despite the fact that she’d just received earth-shattering news, the consultant advised her to continue working as it would take a week for the results to come through.
“People were coming into the pharmacy and I was walking round in a daze,’ she said. “Then, one day I got a phone call to go home as it had been confirmed that I had oesophageal cancer.
“After that, life was just a whirlwind of tests, scans and waiting on results. Waiting for the results was actually the worst thing. We decided not to tell our daughter because we were in the middle of the pandemic and I wasn’t going to put an eight-year-old through any more.
“I had to have chemotherapy to reduce the size of the tumour and I was immediately concerned that everything would be thrown up into the air with the pandemic. Fortunately, I was able to get four cycles of chemotherapy, then had my surgery and then another four cycles: a sort of ‘mop-up’.
“I had the four slots in March and April, and then in May I had to build myself back up for surgery on 16 June. They told me I’d be in ICU for three days, but I was in overnight and back onto the ward the following day. I remember joking with the doctor about making history for getting out faster than anyone! I was in and out in the week and I was back out walking six weeks after the surgery.
“I think that, when it comes to cancer treatment, you have to push your limits to get on with it. I always knew the second cycle of chemotherapy would be bad; the first one nearly killed me and I nearly gave up. There was also the possibility of spread to the lymph nodes, so, instead of giving me false hope, the doctors said they thought it had. But after surgery they tested all the lymph nodes – about 17 of them – and not one of them was cancerous. I was overwhelmed by that. I heard that I had to do another four but it was entirely up to myself. I’m glad I did the whole range because now I know that I can look back and say, I did everything I could”.
“When I heard that my tumour was only one millimetre away from the cavity wall, I knew that someone had been looking down on me. One millimetre is a wee dot. If it had got in there, I wouldn’t have been eligible for surgery.”
Following her surgery and chemotherapy, Leanne’s family and friends rallied around to help her.
“My support has been incredible,’ she said. ‘Absolutely amazing. My husband, Brian, took time off work and my mum took ten months off. Our daughter has been home the whole time and the school worked with me to help her.
“I think the pandemic worked in my favour because no one could carry germs to me and it also brought mental benefits in that I didn’t have to keep having the ‘cancer conversation’ with everyone.”
Working in the pharmacy has convinced Leanne that pharmacists and their teams have a role to play in spotting the signs of potential oesophageal cancer.
“We all notice people coming in and buying reflux and heartburn remedies on a regular basis, so it may be an idea for pharmacists advising someone who repeat buys to ensure they have a diagnosis from their GP rather than self medicating and ignoring symptoms.
“Cancer is a scary word to hear, but if it’s caught early, there are a lot of treatment options available now. There is light at the end of the tunnel, but it’s all about getting it early and knowing your body. You just have to suck it up and get on with it. Take it on the chin.
“I’m so thankful for being given a second chance. It’s been a hell of a roller coaster, but I’ve had more good days than bad days.”
For further information go to ogcancerni.com, follow #OGCancerNI, call 07568 157450 or make an appointment to see your local GP today.